Antibiotic Resistance: A Growing Global Health Threat
Introduction
Antibiotics have been one of the most important medical discoveries in human history. Since their widespread use in the 20th century, they have saved millions of lives by effectively treating bacterial infections that were once fatal. However, the power of antibiotics is now under serious threat due to a phenomenon known as antibiotic resistance. This growing global problem is making common infections harder to treat, increasing medical costs, prolonging hospital stays, and raising the risk of death.
Definition
Antibiotic resistance is the ability of bacteria to survive and continue to grow despite the presence of antibiotics designed to kill them or stop their growth. It occurs when bacteria change through genetic mutations or by acquiring resistance genes, often due to the overuse or misuse of antibiotics, making common infections harder to treat and increasing the risk of disease spread, severe illness, and death.
What Is Antibiotic Resistance?
Antibiotic resistance occurs when bacteria change in ways that reduce or eliminate the effectiveness of antibiotics designed to kill them or stop their growth. Instead of being destroyed, resistant bacteria survive, multiply, and continue to cause infection. As a result, standard treatments become ineffective, and infections persist or worsen.
It is important to note that humans do not become resistant to antibiotics – bacteria do. When antibiotics are misused or overused, they create selective pressure that allows resistant bacteria to thrive while susceptible bacteria are eliminated.
How Does Antibiotic Resistance Develop?
Antibiotic resistance develops naturally over time as bacteria evolve, but human activities have significantly accelerated this process. The main contributing factors include:
1. Overuse of Antibiotics
One of the leading causes of antibiotic resistance is the overprescription of antibiotics. Antibiotics are often used even when they are not necessary, such as for viral infections like the common cold or flu, against which antibiotics are completely ineffective.
2. Incomplete Courses of Treatment
When patients stop taking antibiotics before completing the prescribed course, some bacteria may survive. These surviving bacteria are often stronger and more resistant, increasing the likelihood of future infections that are harder to treat.
3. Misuse in Agriculture
Antibiotics are widely used in livestock farming to promote growth and prevent disease in healthy animals. This practice contributes significantly to the development of resistant bacteria, which can spread to humans through food, water, and the environment.
4. Poor Infection Control
Inadequate hygiene, sanitation, and infection prevention measures in hospitals and communities allow resistant bacteria to spread more easily from person to person.
Why Is Antibiotic Resistance Dangerous?
Antibiotic resistance poses a serious threat to global health, food security, and development. Some of the major risks include:
Increased Mortality and Morbidity:
Infections caused by resistant bacteria are more difficult to treat and often require stronger, more expensive, or more toxic medications. In some cases, no effective antibiotics remain, leading to increased death rates.
Longer Hospital Stays:
Patients with resistant infections often require longer hospital stays, additional tests, and more intensive care, putting a heavy burden on healthcare systems.
Threat to Medical Procedures:
Many modern medical procedures, such as surgeries, organ transplants, chemotherapy, and neonatal care, rely on effective antibiotics to prevent and treat infections. Antibiotic resistance makes these procedures riskier and potentially life-threatening.
Economic Impact:
Antibiotic resistance leads to increased healthcare costs due to prolonged illness, additional treatments, and lost productivity. It is estimated to cost the global economy billions of dollars each year.
Examples of Antibiotic-Resistant Bacteria
Several dangerous bacteria have already developed resistance to multiple antibiotics, including:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant tuberculosis (TB)
- Vancomycin-resistant Enterococci (VRE)
- Carbapenem-resistant Enterobacteriaceae (CRE)
These infections are difficult to treat and are responsible for thousands of deaths worldwide every year.
What Is Being Done to Combat Antibiotic Resistance?
Addressing antibiotic resistance requires coordinated global action. Governments, healthcare professionals, researchers, and individuals all have a role to play.
Surveillance and Research:
Health organizations worldwide are monitoring resistant infections to track trends and identify outbreaks. At the same time, researchers are working to develop new antibiotics, alternative treatments, and rapid diagnostic tools.
Antibiotic Stewardship Programs:
Hospitals and clinics are implementing antibiotic stewardship programs to ensure antibiotics are prescribed only when necessary and used correctly.
Regulations in Agriculture:
Many countries are introducing stricter regulations to limit the use of antibiotics in animal farming, especially for non-therapeutic purposes.
Public Awareness Campaigns:
Educational campaigns aim to raise awareness about the responsible use of antibiotics and the dangers of resistance.
What Can Individuals Do?
Everyone can help slow the spread of antibiotic resistance by taking simple but important actions:
- Use antibiotics only when prescribed by a qualified healthcare professional
- Always complete the full course of antibiotics
- Never share antibiotics with others
- Do not use leftover antibiotics
- Practice good hygiene, such as regular handwashing
- Get vaccinated to prevent infections and reduce the need for antibiotics
By making informed choices, individuals can help preserve the effectiveness of antibiotics for future generations.
The Future of Antibiotics
The rise of antibiotic resistance is one of the greatest public health challenges of our time. While scientific advances continue to offer hope, the development of new antibiotics has slowed, making it even more important to protect the ones we already have.
Without urgent and sustained action, antibiotic resistance could return us to a time when minor infections and routine surgeries become life-threatening. However, through responsible use, strong policies, continued research, and global cooperation, it is possible to control this threat.
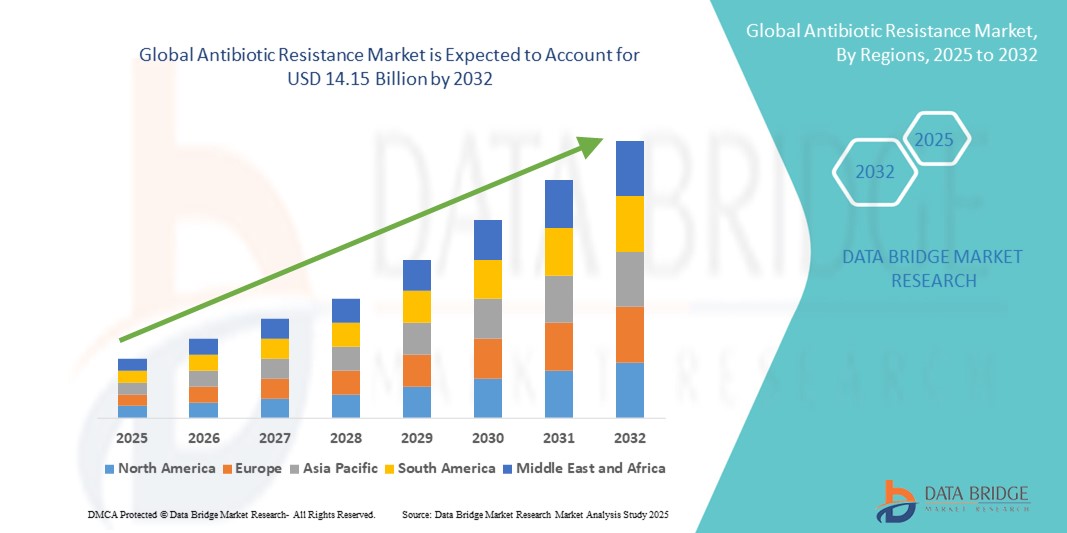
Growth Rate of Antibiotic Resistance Market
According to Data Bridge Market Research, the antibiotic resistance market was estimated to be worth USD 9.08 billion in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 5.70% to reach USD 14.15 billion by 2032.
Learn More: https://www.databridgemarketresearch.com/reports/global-antibiotic-resistance-market
Conclusion
Antibiotic resistance is a complex and evolving problem that affects everyone, regardless of age, location, or lifestyle. Antibiotics remain a precious and limited resource, and their misuse puts global health at risk. By understanding the causes and consequences of antibiotic resistance and taking collective action, we can help ensure that these life-saving medicines remain effective for generations to come.

